Everyday sixteen women die giving life and many more newborns do not live beyond the first 28 days of their lives due to preventable causes, while use of antenatal, natal and post-natal services also remains low.
“One of the barriers to seeking maternal health care and family planning services is the high out -of -pocket expenditure for especially the poorest of the poor including adolescent and young people,” says UNFPA Country Representative Alain Sibenaler.
“Utilization of antenatal, natal and post-natal services has remained low because many couples cannot afford to meet the cost for these services especially the poorest of the poor,” he said.
Ugandans spend 41 percent of their earnings on health care, according to the National Health Accounts Report (2013-2014). The low health financing has also led to high out-of-pocket expenditure in a country where 69 per cent of households depend on substance farming as their main source of livelihood, according to the Uganda Population and Housing Census Report (2014).
Speaking during a meeting with Parliamentarians on the National Health Insurance (NHI) Bill, the Country Representative said, if passed in to law will become a scheme aimed at improving health financing and promoting universal health coverage.
Organized by the Partners in Population and Development Africa Regional Office (PPD ARO) with support from UNFPA, the meeting that took place at Imperial Royale Hotel in Uganda’s capital Kampala aimed to discuss the place of Family planning and Reproductive Health in the Bill.
Family planning uptake in Uganda remains low. According to the Uganda Demographic and Health Survey (UDHS) 2016, 28 percent of women who would like to space or delay child birth do not have access to family planning services.
The report also shows that only 39 per cent of married women are using a method of family planning. Yet again, the report reveals, “contraceptive use increases with wealth....”
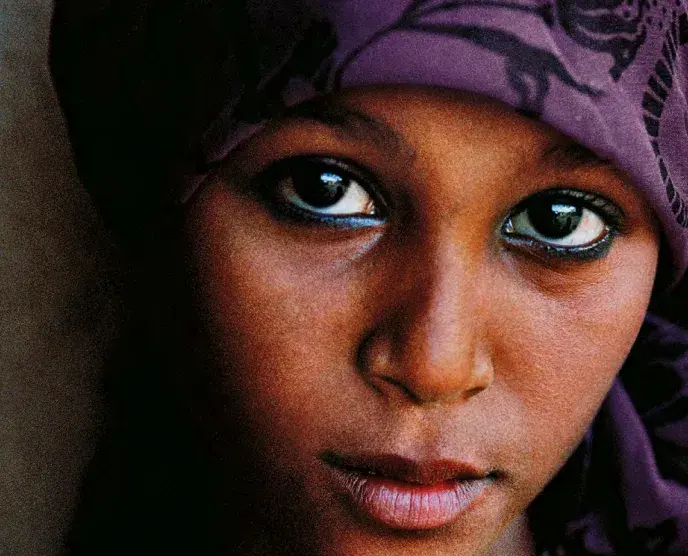
Lack of access to family planning services is also one of the factors leading to high teenage pregnancies with one in every four girls being pregnant or has already had a child by 19 years, the UDHS says.

Therefore, if well designed and implemented, it is hoped, the proposed National Health Insurance Scheme (NHIS) will be a significant step in terms of addressing these barriers, by being all-inclusive and narrowing the social inequality gap, while increasing the number of people accessing quality health care.
“It will enhance health- seeking behaviour and complement efforts to Universal Health care coverage in the country. This in turn will drive us to achieving Goal three of the SDGs to “ensure healthy lives and promote well-being for all at all ages,” and reduction in maternal mortality and New born morbidity and mortality,” Sibenaler said.
However, the Representative added, while NHI is a huge step in the right direction for the realization to the right to health, “we should ensure that we leave no one behind.”
Shortages in health sector personnel should also be averted by training and retaining more health workers including midwives who do not only ensure safe births but also provide family planning and other reproductive health services, he said.
Member of Parliament Beatrice Rwakimari agreed, urging Parliamentarians to continue advocating for an increase in the health budget. In April 2001, the African Union countries pledged to set a target of allocating at least 15 percent of their annual budget to improve the health sector. The national health budget allocation currently stands at 6.4 per cent, which is less than agreed in the Abuja Declaration by heads of African states.
“The issue of the health budget is an issue of concern. Because of this Uganda is facing shortages and flight of human resource,” she said.
Sustainable Development Goal three provides for healthy lives and promotes well-being for all at all ages and emphasizes all aspect of health including reduction in maternal mortality, increasing skilled attendance, ending preventable death of newborns and children below five years and ending the HIV epidemic.
The Uganda Constitution (1995) also provides that “the state shall protect women and their rights, taking into account...their maternal functions…”
UNFPA’s interventions

UNFPA supports the Parliamentary Forum on Population and Development and the Network for African Women Ministers and Parliamentarians (NAWMP) continuous advocacy role on maternal and sexual reproductive health and rights.
Through this effort, over the years, there has been marked increase in budget appropriation and positioning of maternal health, family planning and sexual reproductive health issues in the Parliamentary agenda.
The strong lobbying mechanisms by the Parliamentarians that has resulted in establishing of a conducive policy environment and contributed to the reduction in Maternal and Newborn mortality indicators (from 438 to 368 ) as registered in the UDHS of 2011 and 2016 respectively.
“We have seen improvements in the Reproductive Maternal and Newborn and Child Health indictors as reflected in the preliminary results of the Uganda Demographic Health Survey (2016). Our focus should be improving quality of care at all levels,” Sibenaler said.
Addressing barriers
Once tabled in Parliament, the support of Members to passing of the Bill will be a key milestone in further improving access to and utilization of sexual reproductive health services that will impact positively on maternal newborn health outcomes.
Universal access to family planning will not only help Uganda’s efforts in accelerating social economic transformation to harness a Demographic Dividend through accelerating fertility decline and enhancing investments in family planning, but will also reducing unmet need to family planning to 10 percent and increase modern contraceptive prevalence rate among married women to 50 percent by 2020.
This will also go a long way in fast-tracking attainment of the middle-income country status as envisioned by the Country Vision 2020 and the Uganda Family Planning Costed Implementation Plan (2015-2020).