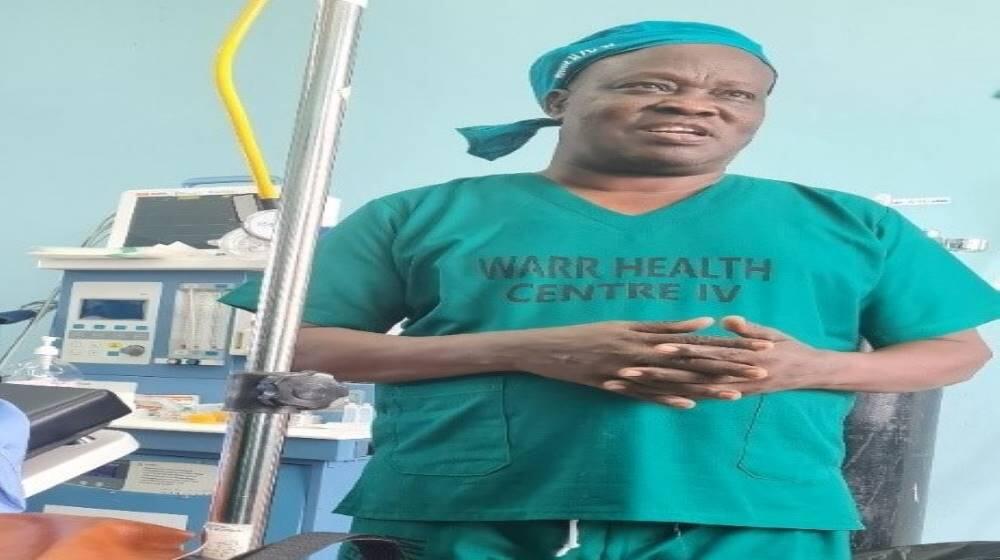
Zombo district, West Nile, Uganda – Dr. Emintone Ayella Odong, Senior Consultant Obstetrician and Gynecologist at Gulu Regional Referral Hospital in Northern Uganda, Dr. Emanuel Odar, Consultant Obstetrician and Gynecologist at Arua Regional Referral Hospital in the West Nile region of Uganda, and Dr. Innocent Waromu, a trainee on fistula repair based in Warr Health Centre IV, Zombo district are some of the unsung heroes in the fight against obstetric fistula. We met this trio at Warr Health Center IV in Zombo district, West Nile of Uganda. They were just concluding their lunch break, about to set off for their afternoon fistula repair session. It was the fourth day of the fistula repair camp that would last five days. That Thursday afternoon, they were setting up for their twenty-first and twenty-second fistula repair sessions.
“We have been here at Warr Health Center IV since Monday, we reviewed 35 cases and 28 were listed for repair,” said Dr. Odong. “We have repaired 20 women so far, and we hope by close of the camp tomorrow, we shall have repaired all of them.”

Dr. Odong explained that obstetric fistula is a hole between the birth canal and bladder or rectum, often caused by prolonged, obstructed labour without access to timely, high-quality medical treatment.
“Fistula takes away the dignity of a woman. For example, when she walks, there is a footmark wherever she passes,” said Dr. Odong.
“Some of us have developed a passion to restore this dignity. Unfortunately, the fistula repair surgeons are not many, about 30 are trained but only about half of us are operating. As you can see, we are only two fistula surgeons in the greater North [West Nile and Northern regions of Uganda]” Dr. Odong added.
Mobilizing women for fistula repair
The women who came for the surgical camp were mobilized by the Village Health Teams (VHTs) and they came from Zombo district and beyond. On the fistula ward, an aura of hope filled the room, collectively transmitted by the women who had already undergone surgery, and visibly showing on their faces.
Seventeen-year-old Hope* had gotten her repair a couple of days earlier. She narrated that she got pregnant at age 14, having gotten married a few months earlier. She had dropped out of Primary Three, running away from her father’s home because she was mistreated by her stepmother. First, she lived with her Aunt in Masindi district, Eastern Uganda. Still feeling unloved, she decided to get married to her ‘sweetheart’, who was then 20 years old. Unfortunately, at the time of birth, she could not push the baby. The midwife had to use a vacuum extraction to help her deliver the baby. It was a baby boy, but did not survive. Days later, she realized that she could not control the flow of urine. Her partner abandoned her a few days after she got the problem.
“It haunts me that I got pregnant so early. I used to have painful menses, I was given herbs and instructions not to meet any man,” Hope said.

According to UNFPA, young girls are particularly vulnerable because their bodies may not be ready for childbirth. Worldwide, pregnancy and childbirth complications are the leading cause of death among girls between the ages of 15 and 19.
But obstetric fistula does not discriminate by age. Shamim*, a 30-year-old mother from Zewu Village in Zombo district was another beneficiary of the surgical camp. Shamim narrates that at age 20, she was carrying her first pregnancy. At the time of delivery, they could not afford the transport fare to the health center which was quite a distance from where they lived. So with her partner, they decided to seek the services of a traditional birth attendant. Unfortunately, she got complications during delivery as the baby could not come out. By the time they took the decision to mobilize a motorcycle to rush her to Hoima Hospital, it was quite late. The Caesarian section could not save her baby because it was too tired, Shamim narrowly survived, but with a fistula. This was Shamim’s second repair, to close a minor outlet that would disturb her through the night, as she would wake up wet every morning. Fortunately, her partner is very supportive and they have had three children following the first repair.
What will it take to eliminate obstetric fistula?
Obstetric fistula has all but disappeared in developed countries with quality health care systems and skilled professionals who can perform Caesarean sections. Yet, UNFPA statistics show that an estimated 500,000 women and girls in more than 55 countries throughout sub-Saharan Africa, Asia and the Pacific, the Arab States and Latin America and the Caribbean are estimated to be living with fistula, with thousands more occurring every year.
In Uganda, Ministry of Health statistics show that more than 1500 fistula repair surgeries are conducted annually. However, there is a backlog of more than 75,000 women awaiting obstetric repair.

Dr. Mary Otieno, UNFPA Representative in Uganda recommends strengthening the prevention aspect in addition to repair: “Women should have access to quality and timely health care before pregnancy, including family planning, as well as during pregnancy including, all antenatal care visits. Childbirth should be supported by skilled health workers who will ensure a safe births and the well-being of mother and baby. And lastly, ensuring the prevention of teenage pregnancy as bodies of young girls have not matured to go through the trauma of childbirth.”
“All these are key components of safe motherhood,” Dr. Otieno adds.
*The names of the survivors are concealed to protect their privacy.
Compiled by Prossy Jonker Nakanjako/UNFPA Uganda